The global SARS-CoV-2 reinfection rate was just under 1% as of a year ago, with significant differences by variant, country, and time, according to a meta-analysis of 55 studies on more than 111,000 cases.
Published in BMC Infectious Diseases, the meta-regression analysis by Sichuan University researchers in China included 46 cohort, 6 case-control, and 3 cross-sectional studies on COVID-19 reinfection rates up to March 2023. Reinfections were considered those identified more than 90 days after a primary case. Possible resurgences or vaccine breakthrough infections were not included.
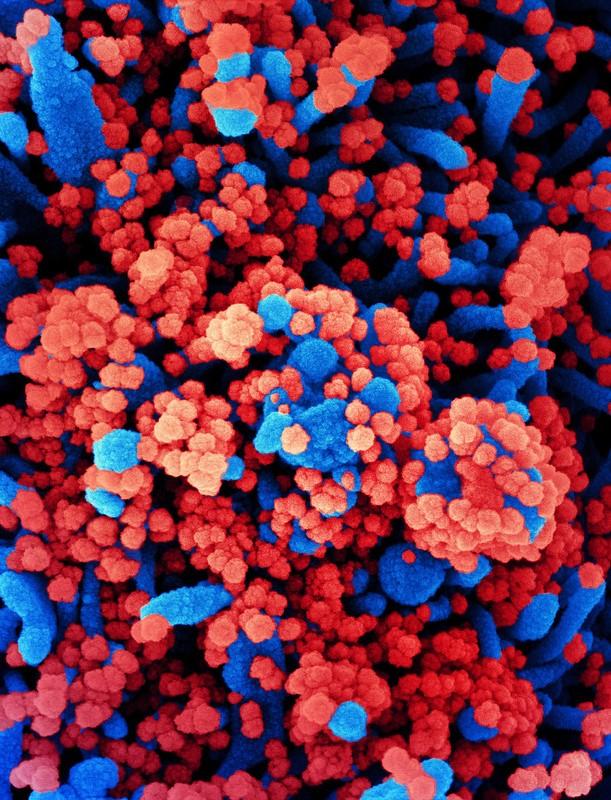
"Reinfections have been reported continuously since the first wave of the COVID-19 epidemic, and especially after the Omicron variant became a major prevalent variant worldwide, there has been a significant increase in the number of reported SARS-CoV-2 reinfections globally," the researchers wrote.
Reinfection rate highest during Omicron
Overall, the COVID-19 reinfection ranged from 0% to 28.4%, and the pooled reinfection rate was 0.9%. There were statistically significant rate differences by variant: 0.3% for the wild-type virus, 0.6% for the Alpha variant, 0.4% for Delta, and 4.1% for Omicron.
Reinfections have been reported continuously since the first wave of the COVID-19 epidemic, and especially after the Omicron variant became a major prevalent variant worldwide.
Brazil had the highest reinfection rate (6.6%), while Spain's rate was 0.3%. The rate varied over time, with the first notable change on day 154 (1.1%). The highest rate occurred on day 361 (2.9%). The US SARS-CoV-2 reinfection rate peaked at 0.2% on day 167.
While the second wave peak was lower than that in the first, the third wave peak was significantly higher. "We speculated that one of the reasons why the third peak was higher than the first peak might be caused by the weakening of the population’s immunity level over time," the authors wrote. "This phenomenon might be due to the fact that immunization levels decreased over time after vaccination or infection with SARS-CoV-2."
"Our results warn us that the natural decay of immune levels over time may lead to the reinfection of SARS-CoV-2, resulting in a new round of COVID-19 pandemic," they added.













